15925 E. Whittier Blvd. Whittier, CA 90603
1 block East of the Whittwood Town Center
Common Eye Conditions
MACULAR DEGENERATION
What causes macular degeneration?
It is most often an age-related disease, commonly diagnosed in people ages 50 and older. A family history of macular degeneration and/or cigarette smoking are also contributing factors.
The two most common types of macular degeneration are dry and wet macular degeneration.
- Dry macular degeneration: This is by far the most common form of the disease. Typically, vision loss is gradual and a person will notice difficulty adjusting to changes in light.
- Wet macular degeneration: Accounting for only ten percent of cases, individuals with wet macular degeneration tend to develop significant vision loss which is often rapid and severe.
What are the symptoms for macular degeneration?
These vary from person to person: sometimes the effects are hardly noticeable, or only one eye is affected. However, when both eyes are affected, the loss of vision is more quickly identified. Look for these symptoms:
- A dark or blank area in your central vision
- Straight lines appear distorted
- When reading, letters or words look blurred
How is macular degeneration diagnosed?
Our physicians and staff conduct a thorough eye examination to test for macular degeneration. This exam will include:
- A dilated exam of your macular using a specialized lens.
- If any sign of macular degeneration is detected, photographs of your eyes may be taken. In addition, a specialized scan of the layers of the retina called
- optical coherence tomography (OCT) may be performed.
How is macular degeneration treated?
Unfortunately, there is no cure or reversal of macular degeneration. However, a large clinical study has proven that taking a multi-vitamin with high levels of zinc on a daily basis can reduce the rate of progression of macular degeneration. Patients can also track their disease at home with an Amsler Grid (which resembles graph paper) and report any changes detected between their regular eye exams.
With wet macular degeneration, most patients receive injections of a drug that can stop blood vessel growth and bleeding. In some patients, laser treatment is also indicated.
DIABETIC RETINOPATHY
What is diabetic retinopathy?
How is diabetic retinopathy diagnosed?
During a medical examination, an ophthalmologist at Marshburn Eye Center will dilate your pupil and look at the inside of your eye with a specialized lens. In this manner, a case of serious retinopathy can often be diagnosed before you are aware of any vision problems. If the doctor diagnoses diabetic retinopathy, he may order color photographs of the retina or a fluorescein angiography to determine if you need treatment.
What is the treatment for diabetic retinopathy?
The best treatment is prevention. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss from diabetic retinopathy. Other treatments include:
- INJECTION of a medication in the eye to reduce selling and shrink abnormal blood vessels may be indicated.
- LASER SURGERY: A laser beam will be focused on different areas of the retina depending on the type of diabetic retinopathy being treated. Be aware that laser surgery does not cure diabetic retinopathy.
- VITRECTOMY: This is a microsurgical procedure that often prevents further bleeding by removing the vitreous gel inside the eye and removes the existing bleeding to improve vision and visual prognosis.
How can I prevent vision loss if I have diabetes?
Schedule regular eye examinations and maintain strict control of your blood sugar.
HOW OFTEN SHOULD I SCHEDULE AN EYE EXAMINATION?
- If you have diabetes, you should be seen by an ophthalmologist at least once a year.
- If you have been diagnosed with diabetic retinopathy, more frequent medical eye exams may be necessary.
- Pregnant women with diabetes should be seen in the first trimester because retinopathy can progress quickly during pregnancy.
- If you are diabetic and need to be examined for eyeglasses, your blood sugar should be consistently under control for several days when you see your ophthalmologist.
- Have your eyes checked immediately if you experience visual changes that affect one or both eyes and last more than a few days, unassociated with a change in blood sugar.
- Upon diagnosis of diabetes, your eyes should be examined within five years if you are 29 years of age or younger, and within a few months of the diagnosis if you are 30 years old or above.
FLASHES and FLOATERS
What are floaters?
A floater is the name given to the small specks or clouds you may see moving in your field of vision. They often present as lines, dots, or dust particles that seem to ‘float’ along with your gaze and are especially noticeable when looking at a plain background, such as a sheet of paper or a blank wall.
Floaters appear to be in front of your eye, but they are actually inside the eye – what you see are the shadows these floating cells cast on the retina (the area in the back of the eye that senses light).
Most people will experience floaters at some point in their lives because they are the result of the eye’s normal aging process. In the majority of instances, floaters are not considered a medical problem and will eventually diminish.
What causes floaters?
Although floaters may appear as specks or cobwebs on the surface of your eye, these particles are actually tiny clumps of cells inside the vitreous (the clear gel-like fluid that fills the inside of the eye). This vitreous gel often starts to thicken or shrink as we approach middle age, forming clumps or strands inside of the eye. When the vitreous gel detaches from the back wall of the eye, floaters appear.
This phenomenon is most common in people who have had YAG laser or cataract surgery; are nearsighted; or have had inflammation inside the eye. However, they can occur in anyone, especially those over 40 years old.
What are flashes?
You may see what appears to be flashing lights, lightening streaks, or light flickers when the thickened vitreous gel has pulled away from the retina. These may be present, on and off, for several weeks or months.
Should I be concerned about my floaters or my flashes?
In the majority of instances, these are not considered a medical problem and require no treatment, although they can be bothersome. Generally, both floaters and flashes will diminish over time.
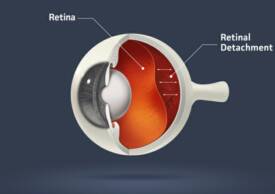
However, the tugging on the retina by the vitreous gel can cause a serious medical problem called a retinal detachment (when the retina tears and actually detaches from the back of the eye).
Symptoms of a retinal detachment include:
- A sudden appearance of floaters and flashes; or a sudden increase in the floaters and flashes you were already experiencing.
- Vision that becomes blurred or distorted.
- A loss of peripheral, or side, vision. This loss may appear like a curtain moving toward the center of your vision with a curved demarcation line. On the inside of the line, the vision is normal, but outside the line, it is dark and gray.
If any of these symptoms occur, contact an ophthalmologist immediately. This could indicate a serious eye emergency. Sometimes flashes of light in the vision can be caused by a migraine phenomenon, but ruling out a retinal cause is important.
How are retinal problems diagnosed?
In our office, an ophthalmologist will dilate your pupil and then use an instrument called an indirect ophthalmascope to examine your retina for any sign of damage. Depending upon the doctor’s findings, he will recommend the appropriate treatment.
How are retinal problems treated?
Torn retina:
With early detection, a torn retina can be repaired with a laser procedure, or with cryotherapy (freezing), which seals the retina to the back wall of the eye. These treatments are performed in the office and cause little or no discomfort. In addition, a retinal tear can be treated using pneumatic retinopexy, an in-office procedure in which a gas bubble is injected inside the eye. This gas bubble pushes the retinal tear back against the eye of the wall, holding the retinal tear closed.
Detached retina:
If a retinal detachment is diagnosed, the only treatment option is surgery. A retina detaches when fluid leaks through a tear beneath the retina causing the retina to lift from the underlying tissue layer. Vision is affected where the retina has separated and this can lead to serious, irreversible vision loss.
At Marshburn Eye Center, an ophthalmologist will examine the characteristic of your detachment before deciding upon the correct surgery for you. Most detachment repair operations are urgent because a detached retina lacks oxygen, which causes cells in the area to die. This can lead to blindness if not treatment immediately. There are several surgeries available to fix a retinal detachment:
- PNEUMATIC RETINOPEXY: Certain types of detached retinas can be repaired using this in-office procedure (see above).
- SCLERAL BUCKLE: At a hospital or outpatient surgery center, a band (called a scleral buckle) is fastened around the eye to pull the retina into place. The scleral buckle bends the wall of the eye inward so that it meets the hole in the retina. This surgery can be performed under local or general anesthesia.
- SCLERAL BUCKLE AND VITRECTOMY: A small instrument is inserted into the eye to remove the vitreous gel contributing to the retinal detachment. When the gel is removed, a gas bubble is put in its place, which pushes the retina against the back wall of the eye.
UVEITIS or IRITIS
What is uveitis?
Uveitis, also sometimes referred to as Iritis, is inflammation of the middle layer of the eye, called the uvea. The uvea is the vascular layer of the eye located between the retina and the sclera (the white part of the eye). The uvea is composed of blood vessels that carry blood flow to the eye and are critical for vision. When this important supply of blood is impaired by inflammation, eyesight may be damaged.
Uveitis can be serious, leading to permanent vision loss. In fact, approximately 10 percent of the blindness in the United States is due to uveitis.
What are the symptoms of uveitis?
Symptoms of uveitis include:
- Redness of the eye
- Blurred vision
- Light sensitivity
- Eye pain
- Dark, floating spots in the field of vision
In many cases, uveitis may develop rapidly: the eye can be red and painful, or vision can be blurred.
In fact, a ‘simple’ case of red eye may be a serious problem of uveitis. If a painful, red eye does not clear up
quickly, consult an ophthalmologist for diagnosis and treatment.
What causes uveitis?
Uveitis has many potential causes. However, in most cases, the cause remains unknown. They include:
- Autoimmune disorders, such as rheumatoid arthritis
- Eye injury
- Infection with a virus, fungus, bacteria or parasite
- Inflammatory disorders such as Crohn’s disease or ulcerative colitis
How is uveitis diagnosed?
A complete eye examination by an ophthalmologist is required to diagnose uveitis. The doctor will examine the inside of your eye and ask about your overall health because uveitis can be associated with disease in the rest of your body.
If you have uveitis, a prompt diagnosis by an ophthalmologist is critical because, when left untreated, uveitis can permanently damage your eyesight and even lead to blindness.
How is uveitis treated?
Because uveitis is a serious eye condition, treatment should begin immediately. Typically, for uveitis not caused by an infection, an ophthalmologist will prescribe eye drops containing steroids to reduce pain and inflammation. In other instances, oral medication or injections may be necessary. Antibiotics are used in patients with infectious uveitis.
Remember that, whatever the course of treatment, it is of utmost importance to seek prompt medical care if you have symptoms of uveitis.
(562) 947-8681
Excellence in Eye Care for over 50 years
What is macular degeneration?
It is a disease of the macula, an area in the retina at the back of the eye which allows you to see fine details clearly. When the macula is not functioning properly, the result is blurry, dark or distorted central vision. Although the central vision is blurred, macular degeneration usually does not affect peripheral, or side, vision. For example, you may be able to see the outline of a person’s face but not be able to discern his or her features.
Macular degeneration is not an easily predictable disease. In some cases, vision is only minimal affected while in other cases vision loss can be rapid and severe. Fortunately, macular degeneration never results in total blindness. Even individuals with the most advanced form of this disease continue to have some useful peripheral vision.
Individuals with diabetes mellitus do not use and store sugar properly. This can affect their eyesight because high blood –sugar levels can damage blood vessels in the retina (the nerve layer at the back of the eye). The damage to these retinal vessels is called diabetic retinopathy. The retina senses light and helps to send imagines to the brain, so when the retinal vessels are impaired, eyesight can be diminished.
In the later and more serious stages of this disease, new blood vessels can grow on the surface of the retina and bleed into the vitreous, thus clouding vision. These blood vessels can also tug on the retina, causing it to detach. If this occurs, surgery is the only viable treatment.
Copyright 2011: Marshburn Eye Center. Eye Doctor Orange County. All rights reserved.
15925 E. Whittier Blvd. Whittier, CA 90603 (562) 947-8681